I was asked to write on prostate cancer prevention for the XY generation, covering anyone born between 1965 and 1990 (aged 33 to 58). According to the latest statistics on SingStat, there are 1.8 million residents in Singapore of that age group. Now, since only half of the population have a prostate (yes if you pee standing, read on..), that is still a sizable 900,000 residents to cover. Yikes!
Unfortunately, as most men need our wives, daughters, partners and maids to take care of us, it still means I will need to reach out to 900,000 men who understand but don’t register and 900,000 women readers who register but don’t understand. Sigh.
Modelling our vaulted education system, I will make understanding prostate cancer as simple and enjoyable as possible so that, at the end of this read, you can answer some basic questions and pass Prostate Cancer 101 with flying colours!
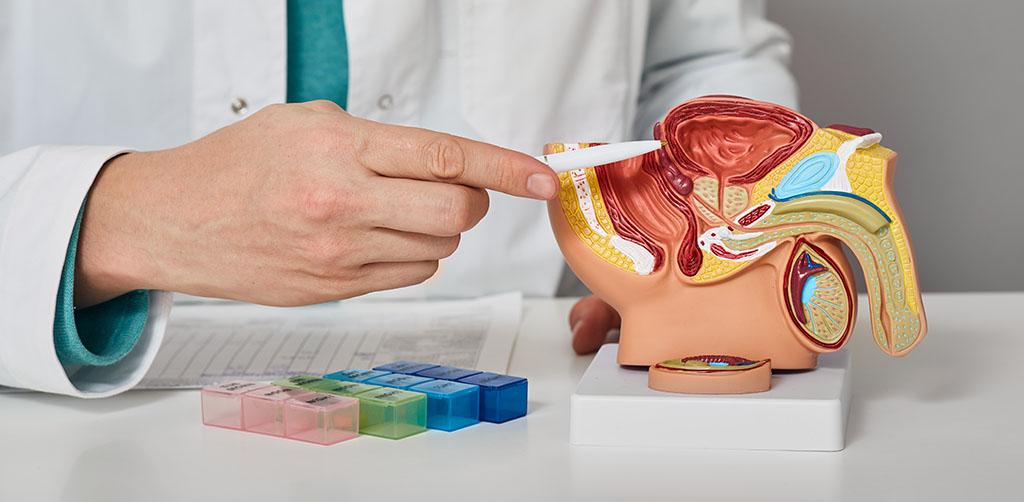
The prostate is a walnut-sized organ that sits at the opening of the bladder and is located between the bladder and the urethra. For most of our lives, it does not bother men as it is deep inside the body. The prostate is crucial to the reproductive system as it provides nourishment to the sperm as it exits our body and allows sperm to live long enough to swim up and fertilise the egg. Without this organ, humans would cease to exist.
Another important by-the-way role of the prostate is that the internal sphincter sits within the prostate (imagine a door that opens and closes), and removing or disturbing the prostate effectively reduces the control men have over the bladder and our reproduction function as sperm flows backwards into the bladder during ejaculation instead of outwards. This is the reason why the prostate is essential, in case you are wondering why we cannot remove it once we finish having kids.
Like any other organ in our body, it can get infected and unhappy at times. Prostatitis is the infection/inflammation of the prostate. It is one of the most common issues that can trouble young men below 50. The symptoms include painful urination, blood in the urine, fever, and a vague tenderness between the perineum (between anus and scrotum). Risk factors for this condition include inadequate hydration, diabetes, urinary stones and, in some cases, sexually transmitted diseases.
If you think you may be presenting symptoms of Prostate Cancer, schedule a consult as soon as possible.
There are four main types of prostatitis, and acute bacterial prostatitis accounts for the majority under 50 years old. While painful, the treatment for this condition is a course of oral antibiotics for two weeks and is self-resolving in most cases.
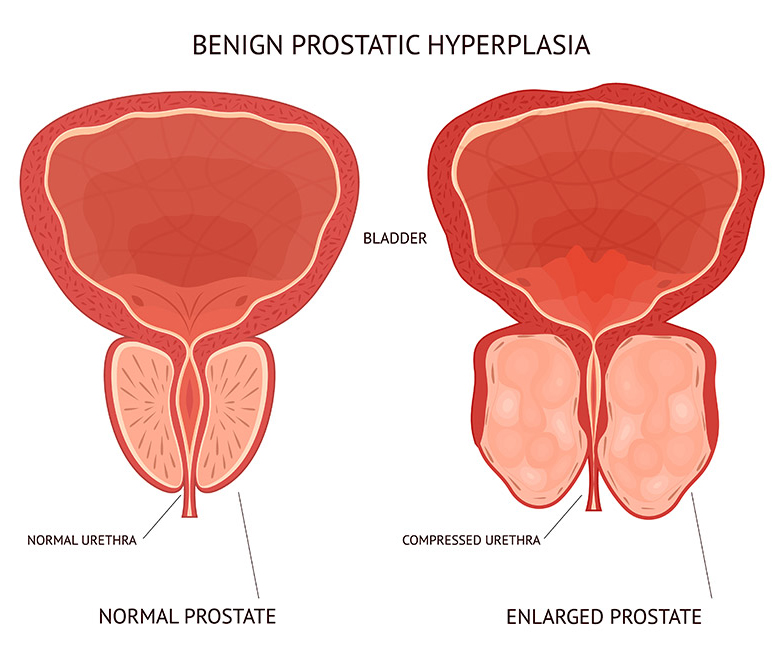
Benign prostate hyperplasia (BPH) occurs when our ever-growing prostate causes the opening of the bladder to narrow and blocks the urine flow. The good news is most of the XY generation would not need to be worried about the prostate as they grow slowly. BPH usually occurs after the age of 50 and may trouble us much later in life when we are in our 60s or later.
In short, under 50, prostatitis or urinary infections are going to be your main issue. BPH symptoms, which include poor flow, terminal dribbling, and nocturia (waking up more than twice at night), can occur starting from 60 years old onwards, while prostate cancer usually affects men over the age of 50.
There will be exceptions to this rule, and it’s always important to see your doctor or (better still) a urologist who specialise in the urinary tract after 45 years old to understand your own body better. In many instances, you are generally lost and forced to backtrack when you or your relatives complain about these sudden discomforts and struggle to figure out who to visit, only to find out there is usually a waiting time involved. Prevention is much better than cure in Urology. Peeing painful, bloody urine is not for the faint-hearted.
Troubling as it is, prostatitis and BPH are benign conditions that can be treated effectively with a whole gamut of lifestyle, oral medications or surgical ways. These diseases can make you very sick, especially if you have other significant medical conditions like diabetes or a smoking history. Prostatitis and BPH can land you in hospital and can even cause death. However, in most cases, if you see a doctor early or have a go-to Urologist, you can resolve the issue quickly and safely.

Prostate cancer is a malignant condition that can creep up to men silently. It was the 3rd most common cancer (incidence) in Singapore between 2010 and 2014 but was the 6th highest cause of death (mortality) in men during the same period. The GEP kids amongst us would have picked up the discrepancy between incidence and mortality. Other cancers like lung and colorectal cancers are ranked 1st/2nd in incidence as well as mortality in Singapore between 2010-2014. In other words, these cancers are deadly and have a universally poor outcome if not diagnosed early. This is not the case for prostate cancer.
The silver lining for prostate cancer is that it is a slow-growing cancer, and even if you are diagnosed with prostate cancer, it is not certain that you will die from it. In fact, it is so slow-growing that a common adage amongst urologists is that we tell patients, “You will die WITH prostate cancer and not FROM prostate cancer”.
Not all prostate cancer requires treatment primarily because it usually presents in your 60s to 80s. If you in your 80s, remain well and not bothered by it (asymptomatic), you can generally leave the cancer alone. Prostate cancer is one of the few cancers in the medical world, that a passive treatment option coined “Watchful Waiting” is featured regularly.
That is not to say that we can ignore this condition, as it is still common enough to cause more deaths than leukaemia, kidney cancers and lymphoma. Hence, the key to surviving your prostate is to find it early and figure out if your prostate cancer is the wolf hiding amongst the sheep.
Before we dive into the topic of taking care of your prostate, it is vital to acknowledge the elephant in the room, i.e. “Can Prostate Cancer be prevented at all?” According to the professional bible that most Urologists in Singapore refer to, the European Association of Urology (EAU) guideline states that “No conclusive data exist which could support specific preventive or dietary measures aimed at reducing the risk of developing Prostate Cancer.”. Certain genetic factors are associated with the risk of aggressive Prostate Cancer, and it is best to speak to your Urologist if you have a family member who has aggressive prostate cancer in their 50s or younger.
For the rest, there are a few ways to monitor the health of your prostate. The most common way of screening is through Prostate Specific Antigen test. PSA is a blood test that measures the level of Prostate Specific Antigen in your body. PSA is a protein that is secreted by both normal and abnormal prostate cells. This blood test is commonly performed as part of health screening packages in the appropriate age group. It is easily performed as it does not require fasting.
PSA can be elevated in BPH, prostatitis and prostate cancer. There is no normal level of PSA as it is a progress measurement of risk; however, 4.0ng/dl is generally accepted as the cutoff between normal and abnormal. An important point to highlight here is that while most commercial labs will highlight values above 4.0ng/dl as red or abnormal, it is not to say that you have prostate cancer, as PSA is a measurement of risk. Similarly, a value of 3.9ng/dl does not guarantee no prostate cancer too. While you may argue that it is a rudimentary interpretation of the cancer marker test for prostate cancer, it is the best (and most established) screening tool we have.
Thankfully, PSA is not the only tool that Urologists depend on to assess your prostate cancer! We employ an even more rudimentary (but time-tested) method to screen for prostate cancer. Unfortunately, due to its location, the prostate is most accessible via the rectum, and DRE is an established component of annual physical examinations for men at risk for prostate cancer. Digital Rectal Examination (DRE) is the most often talked about the part after a visit to the Urologist amongst Singaporean men at the coffee shop and void decks. Some wear it as a badge of honour as the uninitiated cringe while their peers describe the process. This examination is subjected to individual interpretation and is a helpful adjunct if performed by an experienced Urologist.
If your Urologist decides, based on your PSA, DRE and medical history, that there is a risk of prostate cancer, we proceed to the next step of surviving your prostate, which is to perform a prostate biopsy.
If you think you may be presenting symptoms of Prostate Cancer, schedule a consult as soon as possible.
A prostate biopsy confirms the presence of prostate cancer and the grade of the cancer (benign sheep vs dangerous wolf). There are a variety of ways that the prostate can be sampled. In many parts of the world, the prostate is still sampled with a needle via the rectum. A needle is passed through around 12 to 18 times to get prostatic tissue for testing under local anaesthetic. As can be imagined, this route is associated with a risk of sepsis or severe infection due to the presence of stool in the rectum. Apart from infection, trans-rectal ultrasound-guided (TRUS) biopsy is a random process that can miss small cancers as the Urologist is guided by the black-and-white pictures of an ultrasound that does not tell you where the cancer is located.
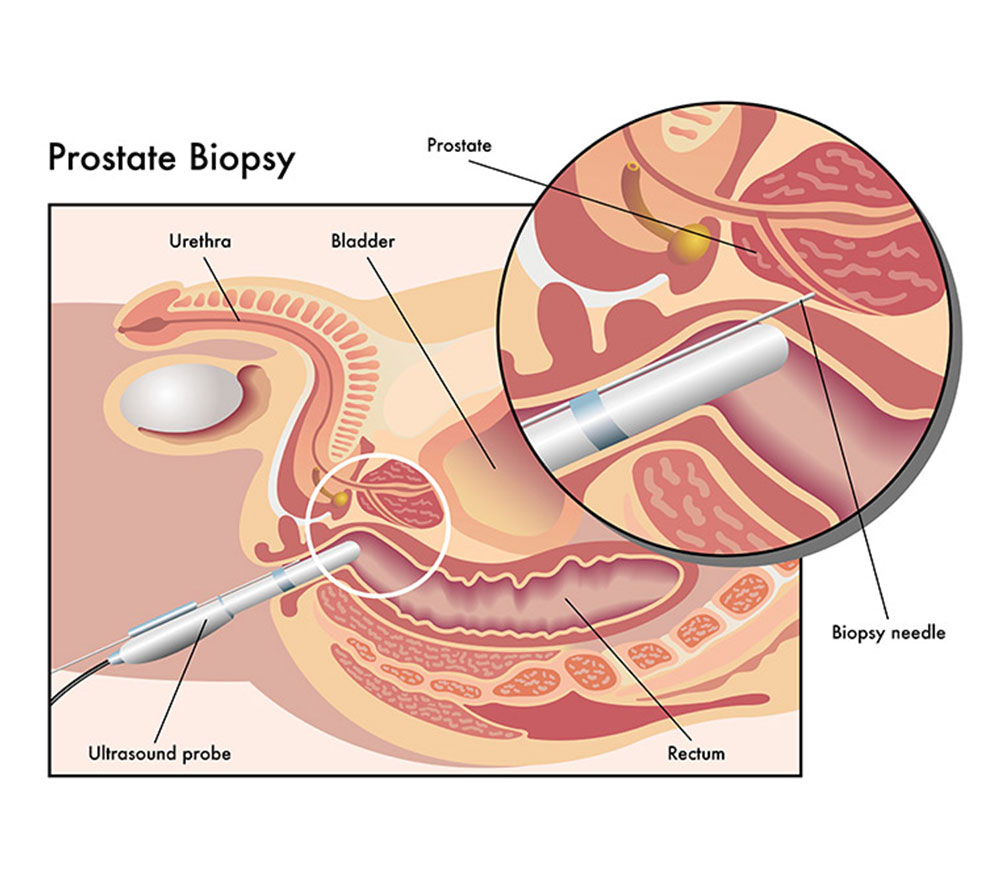
In recent years, there has been a move toward image-guided biopsy of the prostate. Before any biopsy, Magnetic Resonance Imaging (MRI) of the prostate is performed as the first step. MRI prostate grade regions within the prostate using the PIRADs 3-5 grading. The higher the grade, the more likely the presence of abnormality within the specific region.
Imagine going into battle without knowing where the enemy is and carpet bombing mindlessly in the general direction. With an MRI prostate as a guide, we know where the enemy is and can attack a particular region specifically. There are a variety of imaging-guided prostate biopsy platforms regularly in use, as we do not use TRUS-guided biopsy in private hospitals.
I prefer the Biobot platform, which was developed locally by my alma mater, Singapore General Hospital, for which I have direct access to the engineers locally. This MRI-guided robotic system allows me to plan my biopsy purposefully. It is simple to use and will enable me to get to within 1-2mm of my intended target due to experience. Most importantly, the biopsy needle for this platform goes through the skin instead of the rectum and makes two little holes on either side of the perineum. Whether it is 10 or 20 biopsies, you only need a single puncture on the skin, which is dressed with a simple plaster. Minimal infection risk, targeted biopsies and many more areas of the prostate is sampled as you can take up to 50 cores under General Anesthetic, which reduces missed lesions. As the biopsy is performed as a day procedure, you will be discharged home on the same day!
The biopsy is processed, and results are usually available after a week. Our Pathologist colleagues will review the biopsy and give an all-clear or score your prostate cancer between 6 and 10, which indicates the aggressiveness of the lesion.
If the diagnosis of prostate cancer is confirmed, my practice is to go through the results with my patients patiently within the context of prostate cancer. It is important to reiterate that prostate cancer is a slow-growing cancer and that it becomes a team effort to overcome this challenge. Team “We” (patients and I) can have discussions back and forth before deciding on a treatment course. Family members are invited to sit in at the next session with a list of written questions. There is no one-size-fits-all plan, as everyone is different.
Together with your PSA and biopsy grading, additional scans will be required to accurately ‘stage’ your scan. Staging is a necessary step in the management of cancers. It informs me of the degree of spread of the disease at the point of diagnosis. Staging is typically divided into stages 1 to 4. Stage 4 is the most advanced (the stage where sobbing in a drama starts).
There are a variety of treatments available in the armamentarium of a urologist when it comes to prostate cancer treatment. It can range from Active Surveillance to Robotic Surgery, from Watchful waiting to Palliative trans-urethral resection of the prostate (TURP). The final decision is best appreciated through answering a 3-question rule-based approach. Does it need treatment? Is the treatment curative? Does the treatment outweigh the harm that the disease will likely post? Only a limited permutation exists, and I will recommend the treatment plan to the patient, who makes the final decision based on his personal preference and beliefs.
The final decision is individualised and tailored to the person in front of me in consultation with the best available evidence-based medicine and the agreement of the patient’s loved ones. Regardless of the decision and outcome, my patient is guaranteed to have me walking their cancer journey together henceforth.
Our friendly team is looking forward to serving you. For urgent enquiries and appointment requests, please call the clinic directly.

Dr Jay Lim is a urologist with a focus on providing personalised treatment plans specific to your unique urinary and reproductive health needs.

Share this website